Yoga has very much become a familiar aspect within the health and fitness industry. While many practice yoga in order to relieve stress, anxiety and to improve their overall wellbeing, a number of medical studies show that yoga therapy can work to reduce pain. In fact, it has even been proven to improve function in those that suffer with chronic lower back pain. Chronic lower back pain refers to an ongoing pain that lasts longer than three months and is notoriously problematic to treat. Backed by science, many are turning to Iyengar yoga for their back pain. If you’re at the start of your journey with this incredible practice, take a look at sequences of Iyengar yoga poses for beginners, and explore its incredibly powerful healing benefits for yourself.
Learn more about the positive effects of Iyengar Yoga for lower back pain
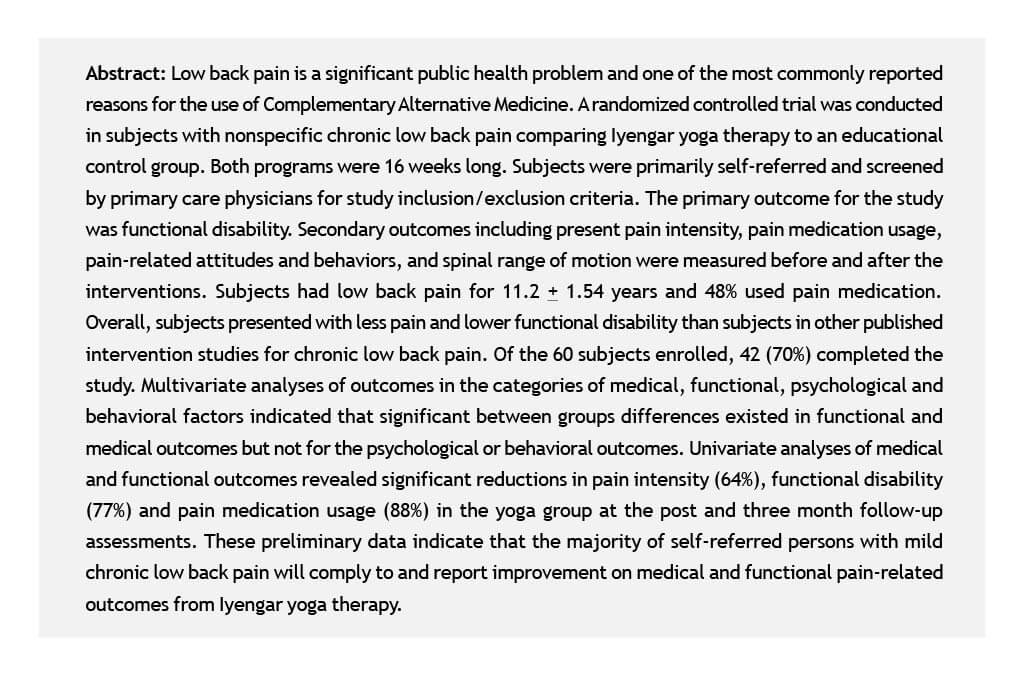
Low back pain (LBP) is a public health problem that has reached epidemic proportions (Shelerud, 1998). In the US, 70-85% of the population has had at least one episode of back pain sometime in their life (Andersson, 1999). LBP is one of the most commonly reported reasons for use of Complementary Alternative Medicine (CAM) (Eisenberg et al., 1993; 1998). An estimated 14.9 million Americans practice yoga, 21% of which use it for treating neck and back pain (Saper et al, 2002).
Ashtanga yoga is comprised of 8 limbs including moral injunctions, rules for personal conduct, postures, breath control, sense withdrawal, concentration, meditation and self-realization (Taimini, 1986). Of the many styles of yoga taught in the US, Iyengar yoga is the most prevalent (Signet Market Research, 2000). It is based on the teachings of the yoga master B.K.S. Iyengar, (1976) who has taught yoga for 70 years and has applied yoga to many health problems including chronic low back pain (CLBP). Although his system descended from Ashtanga Yoga, it is distinguished from other styles of yoga by the emphasis on precise structural alignment, the use of props, and sequencing of poses, and by the incorporation of all aspects of Ashtanga Yoga into the practice of postures and breath control (Iyengar, 1989). Iyengar yoga was chosen for this study because a high prevalence of Americans practicing Iyengar yoga (Signet Market Research, 2000) and the expectation of yielding the best possible outcome. The method is supported by a national credentialing organization with high teaching standards, (IYNAUS Certification Committee 2002) and a standardized protocol for LBP (Iyengar, 1976).
A number of randomized controlled studies exist on the efficacy of yoga. These include osteoarthritis (Garfinkel et al., 1994), carpal tunnel syndrome (Garfinkel et al. 1998), multiple sclerosis (Oken et al., 2004), bronchial asthma (Nagarathna and Nagendra 1985; Vedanthan et al. 1998), pulmonary tuberculosis (Visweswaraiah and Telles, 2004), drug addiction (Shaffer et al. 1997), hypertension (Murugesan et al., 2000), irritable bowel syndrome (Taneja et al., 2004), lymphoma (Cohen et al., 2004) and mild depression (Woolery et al., 2004). Four of these studies evaluated Iyengar yoga (Garfinkel et al., 1994, 1998; Oken et al., 2004; Woolery et al., 2004) and reported positive results.
Only three peer-reviewed studies of yoga and CLBP have been published. Two of the studies evaluated an unspecified method of hatha yoga. One study lacked a control group (Vidyasagar et al., 1989) while the other was not powered to reach statistical significance (Galantino et al., 2004). The third was a feasibility analysis of Iyengar yoga presenting only baseline data and adherence rates to therapy (Jacobs et al., 2004).
Although the therapeutic application of Iyengar yoga for CLBP is currently offered at Iyengar Yoga Centers, there has been no published scientific evaluation of the intervention. The purpose of this exploratory study was to determine the efficacy of Iyengar yoga therapy on pain-related outcomes in persons with CLBP. It is hypothesized that the yoga therapy group will report a greater reduction in a number of pain-related measures.
Method
Subjects
The study was approved by the Institutional Review Board at West Virginia University. Subjects were recruited through physician and self-referral. Local physicians were informed about the study through lectures and mailed announcements. The project was announced to the public through flyers, public radio, and local university list serve for faculty and staff. The inclusion criteria were: history of nonspecific LBP with symptoms persisting for > three months. Subjects had to be > 18 years of age, English-speaking, and ambulatory. Individuals were excluded if their LBP was due to nerve root compression, disc prolapse, spinal stenosis, tumor, spinal infection, alkylosing spondylosis, spondylolisthesis, kyphosis or structural scoliosis, or a widespread neurological disorder. Individuals were excluded if they presented as pre-surgical candidates, were involved in litigation or compensation, displayed a compromised cardiopulmonary system, were pregnant, had a body mass index > 35, were experiencing major depression or substance abuse and were practitioners of yoga. Eligibility also was contingent on subjects’ agreement to randomization and to forgo other forms of CAM during the study.
Study Design
During the pre-intervention assessment, subjects signed an informed consent and completed a battery of psychosocial questionnaires, and spinal range of motion (ROM) measurements. Data collectors were blind to the subject’s treatment status. Subsequently, subjects were randomized to control or yoga groups using a random number generating program from JMP 4.0 statistical software (SAS, 2000; see Figure 1). Randomized subjects were assigned to one of three subgroups of 10 (i.e., Groups I, II, and III) during the fall 2001 and spring 2002 based on the date of their enrollment. Both groups received 16 weekly newsletters on back care written by senior entry level physical therapy students while also being permitted to continue medical care for LBP. In the two weeks preceding the start of the program, the control and yoga groups received two one hour lectures of occupational/physical therapy education regarding CLBP. Instructional handouts were given to help subjects use the information they received.
Yoga group subjects were required to attend one 1.5-hour class each week taught by a yoga instructor for 16 weeks at a community yoga studio. Yoga subjects were also encouraged to practice yoga at home for 30 minutes, 5 days per week. Both groups were asked to attend a 1.5-hour post-intervention assessment 16 weeks following the start of the program to complete questionnaires, and spinal ROM measurements. Data collectors were blind to the subject’s treatment status. Three months after program completion, a third battery of questionnaires was mailed to all subjects. Subjects were asked to complete and return the questionnaires in stamped, self-addressed envelopes to the researchers. Results from the post-treatment and three-month follow-up assessments were compared to baseline measurements.
Yoga Therapy Intervention
The yoga therapy intervention is based on the teachings of BKS Iyengar who has taught yoga for 70 years and has applied therapeutic variations of classical poses to many health problems including CLBP (Iyengar, 1976). It was posited that Iyengar yoga therapy would progressively rehabilitate LBP by addressing imbalances in the musculoskeletal system that affect spinal alignment and posture. The wide range of postures and supportive props employed by this method serve to enhance alignment, flexibility, mobility and stability in all muscles and joints that affect spinal alignment and posture. A variety of props are used including sticky mats, belts, blocks, chairs, wall ropes, benches, boxes, stools, trestler and weights. These props are used to provide external support, to facilitate relaxation, to provide traction and to bring awareness to a specific regions of the body. Many muscle groups are targeted by Iyengar yoga with the aim of lengthening constricted or stiff muscles and strengthening core postural muscles that are underutilized including muscles of the abdomen, diaphragm, hamstrings, quadriceps, hip adductors and lateral rotators, buttocks, muscles of the lumbar and thoracic areas of the back.
The yoga intervention was developed with the consultation of senior Iyengar yoga instructors who had experience with B.K.S. Iyengar’s protocol for treating CLBP. The principal investigator, an Iyengar student for 14 years and teacher in training for 9 years, was introduced to the protocol for CLBP by Geeta Iyengar at Ramamani Memorial Institute in Pune, India in 1998. Since then she has utilized this therapeutic protocol and studied under senior Iyengar teachers with a minimum of 25 years of experience.
The yoga instructors have trained in the Iyengar method for over 10 years, teaching yoga for 8 years and have experience teaching persons with CLBP. Although the PI served as one of the yoga instructors, she was not involved in data collection or data analysis of the results.
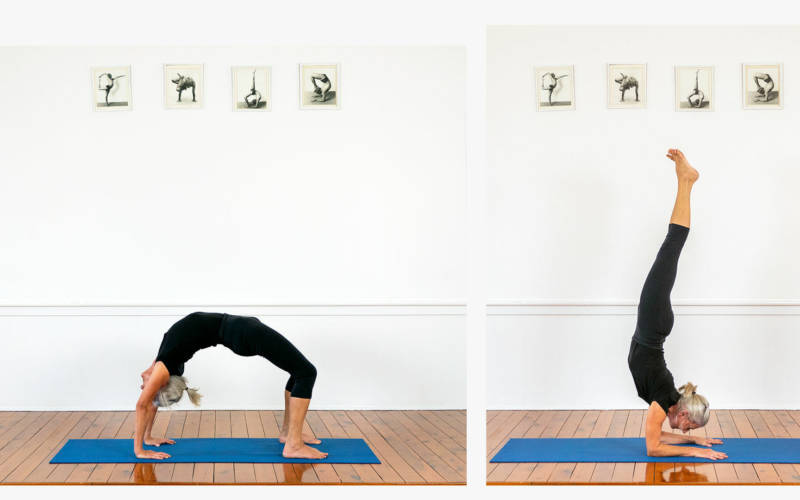
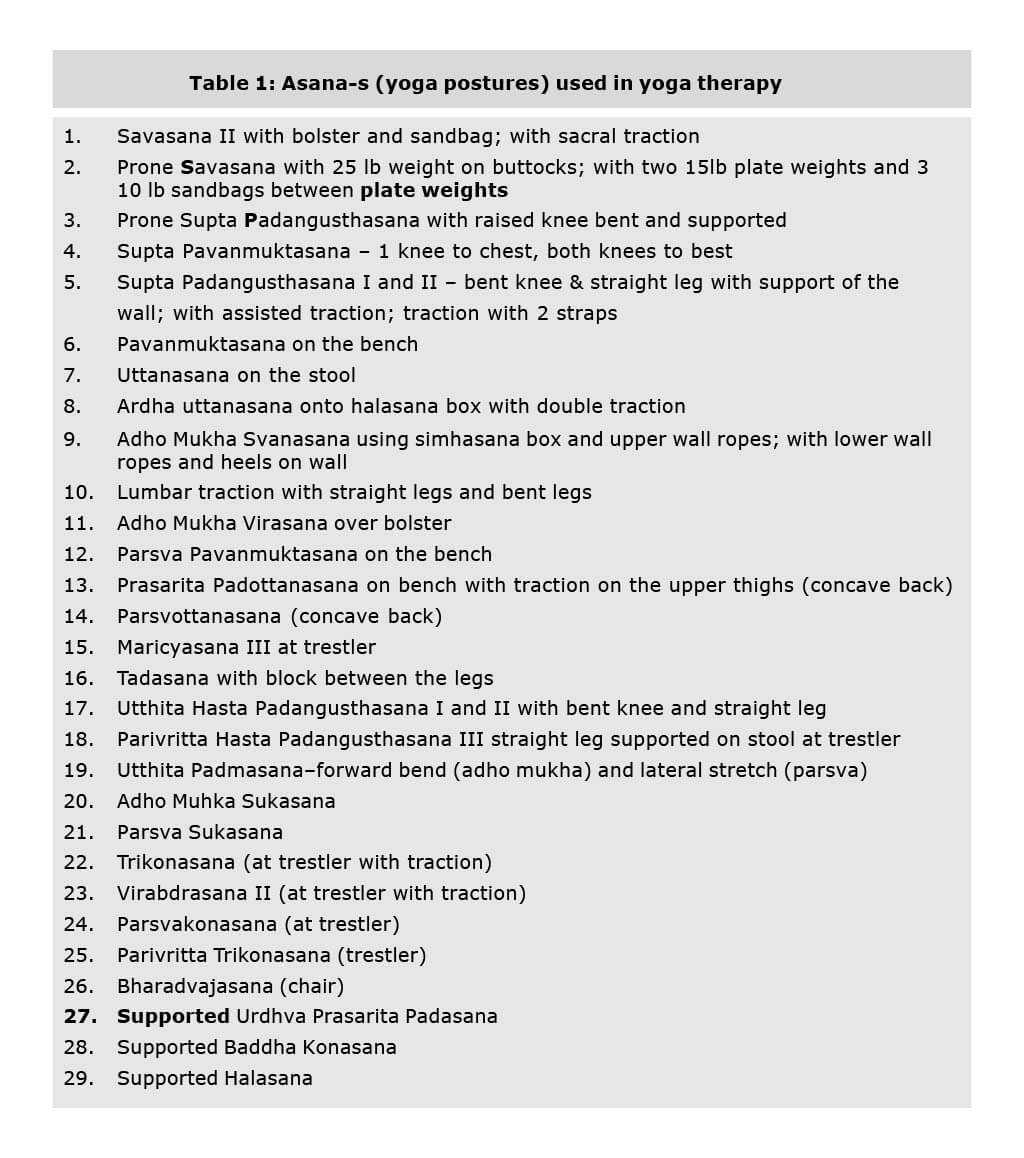
The intervention consisted of 29 postures (see Table1). Poses from the following categories were used: supine, seated, standing, forward bends, twists, and inversions. No back bending poses were introduced at this stage of recovery to reduce the risk of re-injury. Back bending poses require a proper progression of musculoskeletal retraining and can be harmful if done without implementation of complex musculoskeletal actions (Williams et al, 2003). Initially, restorative poses were done to relieve pain and muscle tension. Then poses were introduced that lengthened muscles attaching to the spine and pelvis in positions with the spine fully supported. Next standing poses were introduced to open the hips and groins and to teach students how to use their legs and arms to lengthen pelvic and spinal tissues.
Twists were taught to access the deeper layer of back muscles to help realign the vertebra, increase intervertebral disc space and decrease possible impingement of nerve roots. Inversions were included to reverse the compressive effects of gravity on the intervertebral disc space. Subjects were gradually progressed from simple poses to progressively more challenging poses. Throughout the intervention, instructors focused on correcting imbalances in muscles affecting spinal alignment and posture as they were revealed in the poses. At the program end, yoga subjects were encouraged to continue yoga therapy at home and through community classes.
Outcome Measures
Functional Disability
Functional disability was the primary outcome variable and was measured using the 7-item Pain Disability Index (PDI) (Tait et al., 1990) that assessed the degree (1-10 scale) that chronic pain disrupts performance or function of seven general areas of normal activities including family and home responsibilities, recreation, social activity, occupation, sexual behavior, self-care, and life-support activity (Tait et al., 1990). A total disability score was calculated by summing all items for a maximum score of 70 points with higher scores indicating higher levels of disability. The PDI has been found to be both reliable (Tait et al., 1990) and valid (Jerome and Gross, 1991, Chibnall and Tait, 1994).
Clinical Pain
Clinical levels of pain were assessed using the Short Form-McGill Pain Questionnaire (SFMPQ) (Melzack, 1987). The SF-MPQ measures present pain intensity with a standard horizontal 10 cm visual analogue scale (VAS) (Huskisson, 1983) and the Present Pain Index (PPI) (Melzack, 1987). The VAS is a bipolar line scale with the descriptive anchors of no pain on the left side of the line and worst possible pain on the right side of the line. The PPI is a rating scale from zero = no pain to five = excruciating that requires each patient to endorse their pain with one check.
Fear of Movement
Pain-related fears to movement were quantified by the Tampa Scale of Kinesiophobia (TSK) (Kori et al., 1990, Crombez et al., 1999a; Crombez et al., 1999b; Goubert et al., 2002; Lethem et al., 1983; McCracken et al, 1992; Vlaeyen et al., 1995; Waddell et al., 1993). The TSK is constructed on a 4-point scale with anchors ranging from “strongly disagree” to “strongly agree”. Higher scores are associated with greater pain-related fear of movement (Vlaeyen et al., 1995). Internal consistency of the TSK is fair (alpha = 0.68 and 0.80) (Vlaeyen et al., 1995) while demonstrating good validity among CLBP patients (Crombez et al., 1999a).
Pain Attitudes
Beliefs associated with adjustment to chronic pain were assessed with the Survey of Pain Attitudes (SOPA) (Jensen et al., 1994). The SOPA is a 57-item questionnaire that rates level of agreement on a 0-4 scale with statements concerning perceptions of seven attitudinal areas related to pain including Control, Disability, Harm, Emotion, Medication, and Medical Cure. Higher scores indicate an increase in the beliefs or attitudes that influence chronic pain and disability in a negative way with the exception of the control and emotion subscales. The validity of the SOPA is good (Strong et al. 1992) while demonstrating moderate to good reliability (Jensen et al., 1994).
Coping Strategies
Various coping strategies were assessed using the Coping Strategies Questionnaire – Revised, (CSQ-R) (Robinson et al., 1997; Riley, III and Robinson, 1997). The CSQ-R consists of 27 items and uses a 0-6 rating scale to rate perceived use of six types of coping strategies for pain when pain is experienced including: Distraction, Catastrophizing, Ignoring Pain, Distancing, Cognitive Coping, and Praying. The psychometric properties of CSQ-R are well established (Robinson et al., 1997; Riley, III and Robinson, 1997).
Self-Efficacy
Subjects’ perception of their confidence to actively cope with CLBP at the time of assessment was measured with the Back Pain Self-Efficacy Scale (BPSES) (Anderson et al., 1995). The BPSES presents 22 statements about coping strategies for pain and rates self-efficacy using a 10-point scale from 10 low certainty to 100 totally certain. Higher scores correspond to greater self-efficacy beliefs toward LBP. Three subscales exist including self-efficacy for pain management, functional ability and controlling symptoms. Evidence indicates this scale has good concurrent and construct validity (Anderson et al., 1995) and good internal consistency.
Range of Motion
Spinal ROM was measured using a Saunders Digital Inclinometer, which is a portable, handheld device with a liquid crystal screen that does not require calibration. The curve-angle method for measuring spinal ROM was utilized. The method more effectively isolates ROM of lumbar flexion and extension because it takes into consideration each individual’s different standing lumbar posture in determining its zero reference point for measurements. Testing was performed with awareness of common measurement errors identified by Mayer et al. (Mayer et al., 1997). Assessments were performed in the standing position and included hip flexion and extension, lumbar flexion, extension, and right and left lateral flexion (side bending).
Pain Medication Usage
Subjects were interviewed about their current pain medication usage (within the past 3 months) during the telephone-screening interview. Questions were asked to determine the use of “pain relieving” prescription and nonprescription medications as well as the use of herbal and dietary supplements for pain management prior to the intervention. Changes from the baseline in drug consumption were evaluated at post intervention and at 3-month follow-up. Subjects were given a list of their medications reported at baseline and asked to specify whether there was a change. Responses were coded in either one of four categories: no change from baseline, an increase or a decrease in usage, or cessation of medication. If a subject changed to a drug regimen that was equivalent to the pre-intervention drug regimen with respect to medication class and/or dosing period, and which was expected to yield a similar analgesic response, the drug usage was considered unchanged. Changing the dose or stopping of one or more components of a multiple drug regimen was also considered an alteration in drug usage. For example if two analgesics were being used, and one was stopped, it was recorded as a reduction in pain medication usage.
Adherence
Subjects in the yoga group were asked each week to report the frequency and duration of their yoga therapy practice at home. The total practice time was calculated each week and an average score was determined for the 16 week intervention period.
Statistics
Unpaired t-tests were conducted to determine if baseline differences in demographics, medical history and outcome measures existed between groups. Unpaired t-tests were also conducted to assess whether study completers differed significantly on outcome measures at baseline from non-completers. A non-completer was a subject who either failed to complete the program or failed to complete post-treatment assessment of study outcomes.
Repeated measures mulita-variate analysis was conducted on functional (functional disability and pain intensity), psychological (pain attitudes, fear of movement and self-efficacy), and behavioral (coping strategies) outcomes to control for type I error. For spinal range of motion, only pre and post-intervention scores were obtained and included in the multivariate analysis. If the outcome of the multivariate analysis was significant an ANCOVA was conducted that controlled for baseline scores of study outcomes to assess whether changes from baseline were significantly different between the yoga and control groups at post-treatment and the three-month follow-up. Changes in pain medication usage were analyzed with Chisquared analysis and were assessed for their significance after Bonferroni correction of the significance level for the number of outcomes included in the analysis.
Results
Subject Characteristics
Of 210 candidates who called in or were referred by their physician to participate in the study (Figure 1), 70 (33%) met the inclusion criteria and 60 (29%) agreed to enroll. One hundred forty candidates were excluded before enrollment for the following reasons: logistical conflicts (72.8 %); contraindicated medical conditions (13.6 %); or unwillingness to forgo other forms of CAM (13.6%). Of the 60 subjects starting the study, 42 completed the study giving a 70% completion rate. Ten subjects were excluded from the analysis in the yoga group for the following reasons: 3 for not showing up to intervention after attending the baseline assessment, 3 quit, 1 adverse event in a subject with symptomatic osteoarthritis who was diagnosed with a herniated disc during the study, 2 medically ineligible (pregnant, scoliosis), 1 subject with symptomatic osteoarthritis who was unwilling to perform active yoga postures for fear of aggravating her condition. Review of the adverse event by a medical panel summoned by the Institutional Review Board determined that it was unrelated to the performance of yoga postures. Eight subjects were excluded from analysis in the control group for the following reasons: 4 were lost to follow-up, 2 became ineligible because of other CAM treatment for CLBP, 1 no show at baseline assessment and 1 elderly subject died. Of the 20 subjects completing the yoga intervention, an attendance rate of 91.9% was achieved for the 16-week protocol.
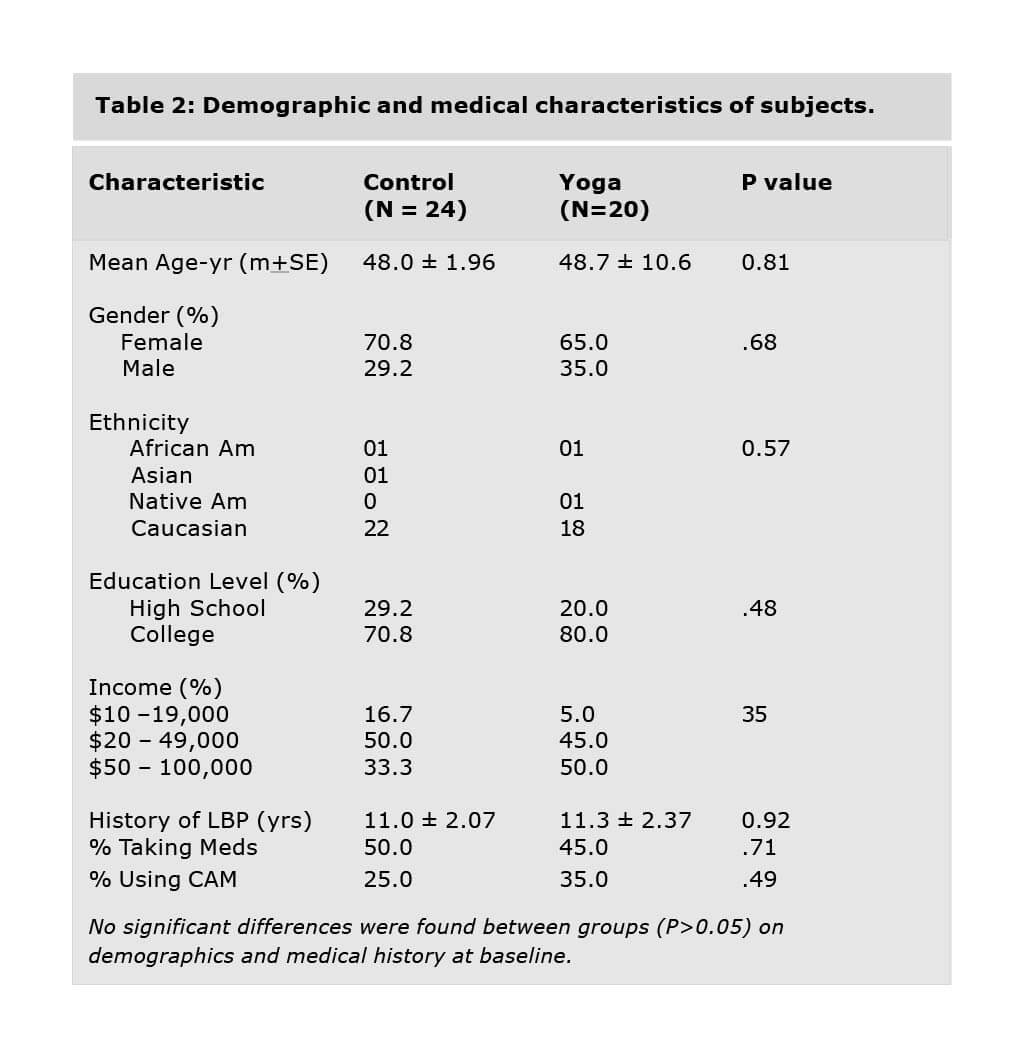
Forty-four subjects (control + yoga) completed the 16-week intervention. The mean age was 48.3 + 1.5 with a range of 23 to 67 years. Subjects reported an average duration of LBP of 11.2 + 1.54 years, 48% reported using pain medication, and 30% used some form of CAM for LBP at baseline (see Table 2). A one-way ANOVA (unpaired t-test) revealed no significant differences in demographics and medical history between the yoga and control groups (P > 0.05; Table 2). No significant between group differences were found at baseline on outcome variables with the exception of significantly higher functional ability on the BPSES (P=0.005), lower catastrophizing as a coping strategy (P =0.007), and less perceived disability (P =0.002) and harm (P =0.02) on the SOPA by the yoga group compared to the control group.
One-way analysis of demographic factors, medical history, baseline pain intensity, and disability comparing subjects who completed the study (N=42) and subjects who either dropped out or were lost to follow-up (n=18), revealed no significant between group differences in demographics, baseline disability or pain intensity. However, non-completers had LBP for a longer period of time (16.4 ± 2.5 yrs.) compared to completers (10.21 ± 1.51 yrs.).
Comparison of Study Outcomes in the Yoga and Control Groups
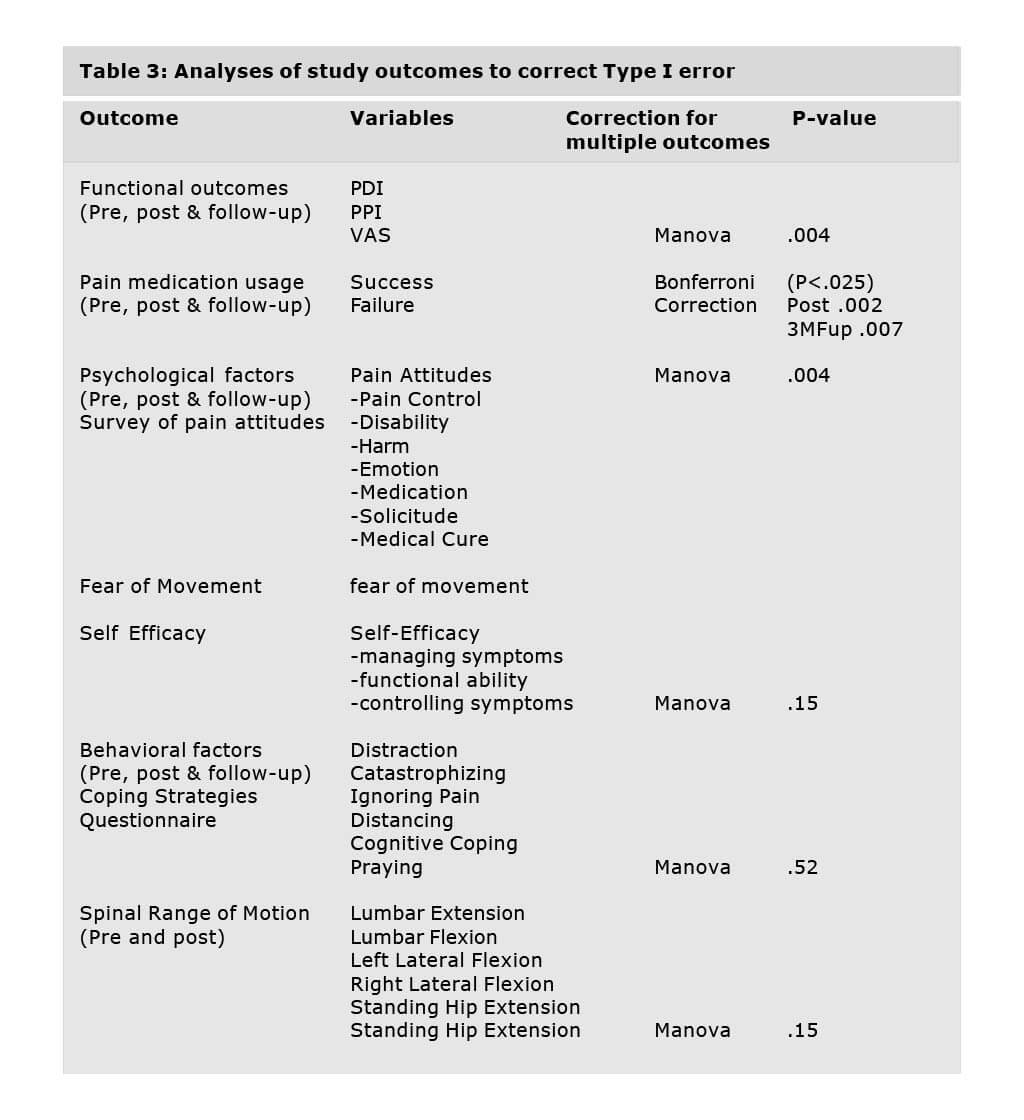
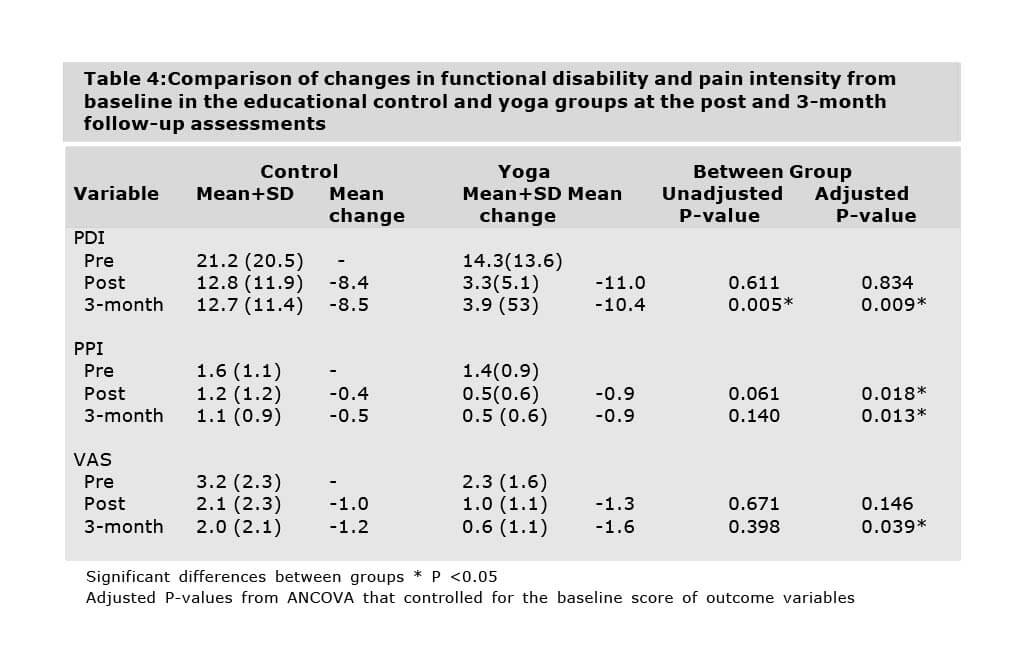
A multivariate analysis of functional, psychological and behavioral outcomes determined that significant group x time differences existed in the primary outcome, functional disability and the secondary outcome, pain intensity (P=.0036; Table 3). No significant differences were found in the other secondary outcomes including spinal range of motion, psychological or behavioral factors. Significant between group differences were observed in the changes in pain medication usage using a Bonferroni corrected significance level. Both the post and three-month follow-up P values were less than the Bonferroni corrected significance level of .025 (Table 3).
Univariate analysis of functional disability indicated that the yoga group has less functional disability post treatment than the control group (Table 4). At baseline, the mean functional disability was 14.3 (13.6) and 21.2 (20.5) for the control group and the yoga group, respectively. After 16 weeks, the mean score fell to 3.3 (5.1) in the yoga group (76.9%) and to 12.8 (11.9) in the control group (39.6%). Three months after the intervention, the mean score was 3.9 (5.3) in the yoga group (72.7%) and 12.7 (11.4) in the control group (40%). A one way ANCOVA that controlled for baseline score, indicated that functional disability was significantly lower in the yoga group compared to the control group (P =0.005) immediately after the intervention. The greater improvement in functional disability by the yoga group was maintained at the three month follow-up (P=.009).
Univariate analysis of present pain revealed that yoga subjects reported two times greater reductions in pain than the control group (Table 4). At baseline, the mean VAS score was 2.3 (1.6) and 3.2 (2.3) for the yoga group and the control group, respectively. After the 16-week intervention, the mean score fell to 1.0 (1.1) for the yoga group (56.5%) and to 2.1 (2.3) for the control group (31%). At the three month follow up, the mean VAS score was 0.6 (1.1) for the yoga group (69.6%) and 2.0 (2.1) for the control group (37.5%). The difference between the two groups became statistically significant at three month follow-up when the yoga group reported a 70% decrease in present pain compared to the 38% reduction reported by the control group (Table 4).
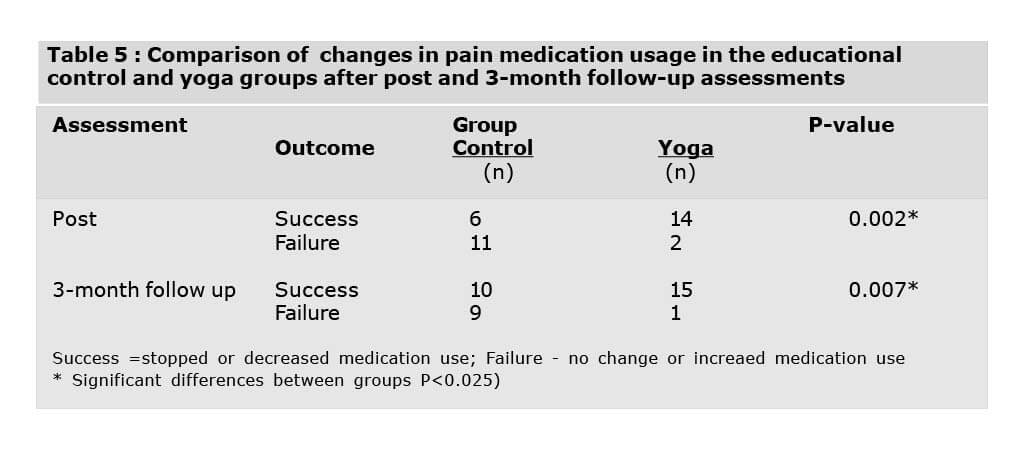
Pain medication was used by 17 of 24 subjects in control and 18 of 20 subjects in yoga. The subjects used non-steroidal anti-inflammatory drugs (NSAIDS) or acetaminophen. However, one participant in the control group also used a narcotic and muscle relaxant while another used only a muscle relaxant. In the yoga group, four subjects reported using muscle relaxants in addition to NSAIDS with one subject using a narcotic occasionally. Drug usage reported immediately following completion of the study treatments decreased significantly in the yoga group compared to the control group (P =0.002) (Table 5). Upon completion of the 16-week intervention, 88% of the subjects in the yoga group reported decreasing or stopping their medication compared to 35% in the control group. One patient in the control group reported an increase in drug use. None of the patients who used a regimen with multiple analgesic medications reported reducing or stopping a pain medication, while increasing another in the regimen. At the three-month follow-up, both groups reported further decreases in pain medication usage, but the yoga group continued to report significantly greater reductions than the control group (P=0.004, Table 5).
An average of the weekly reported adherence to yoga at home indicated that subjects (n=20) in the yoga group who completed the study practiced 52.3 (7.5 min) minutes per week.
A social validation questionnaire was administered at post-intervention and at 3-month follow-up to all subjects for evaluation of potential confounds and to rate perceptions of the efficacy of the interventions. Possible confounds probed included use of medical or non-medical treatment, lifestyle changes, or other activities that could impact their LBP. Non-significant differences were found between groups for the above four areas. In addition, both groups were asked whether they read, implemented suggestions in the newsletters or found the information helpful to their recovery from LBP. Overall, 82.2 % read greater than half of the 16 newsletters distributed (n=37), 68% (n=30) reported implementing between half to all of the suggestions recommended in the newsletters, and 79.5% (n=35) of respondents indicated the newsletters were of some to no importance to aiding in the management and recovery from CLBP. No significant between group differences were found on responses to the above three questions. In the yoga group, 95% of subjects (n=19) rated yoga as having either some (n=2) or a large impact (n=17) on their LBP. Moreover, on a 1 to 5 scale with 1= “no importance” and 5 = “great importance”, 75% respondents rated yoga of great importance (n=15) while the remaining 25% rated yoga as of “some importance.” The entire group rated the yoga treatment as important for managing and recovering from LBP.
Discussion
This is the first study to present results of the efficacy of Iyengar yoga on CLBP using a randomized controlled trial. The results support the hypothesis that yoga therapy confers greater benefits to CLBP patients than an educational program. It was demonstrated that a 16-week yoga therapy intervention caused a significant reduction in self-reported disability and pain, and reduced use of pain medication compared to the group in the educational program. The significant improvements by yoga subjects were maintained at the 3-month follow-up, indicating that the yoga intervention is associated with longer lasting reductions in disability and pain outcomes than an educational intervention.
Since both groups improved after their respective interventions in this relatively healthy population of subjects with CLBP, one possible reason for the reported improvement is regression to the mean.
However, we think this is unlikely since the control group did not show the same degree of improvement and subjects with such a long medical history of CLBP would be unlikely to improve in 16-weeks in the absence of an intervention. In addition, the majority of subjects in the yoga group rated yoga as having a large impact on their LBP and as having great importance to the management and recovery of LBP.
Improvements in several outcome variables compared favorably to similar studies using active treatment strategies such as exercise, physical therapy protocols incorporating flexibility and strengthening exercises, and cognitive behavioral therapy. The reduction in functional disability due to yoga was greater in 4 out of 5 high quality studies of exercise and CLBP (Frost et al. 1995; Kankaapää et al., 1999; (Risch et al., 1993; Torstensen et al., 1998; O’Sullivan et.al., 1997). The reduction in pain intensity due to yoga was greater or equal to the reduction reported in 3 of the 5 exercise studies reported above. The effect size (ES) for functional disability and present pain intensity due to yoga in the current study were 2.6 and 0.5, respectively. These ESs were lower than the ES of the treatment group in the above exercise studies but were similar to or higher than the ES from a meta-analysis of cognitive behavioral interventions for adult chronic pain (Morley et.al., 1999). A large part of the lower ES due to yoga in the current study reflects the much higher changes from baseline in the control group compared to controls in the above exercise studies. In the current study, the ES of yoga on functional disability (Bombardier et al., 2001) but not on pain intensity (Hagg et al., 2003) meets the reported criteria for being minimally clinically significant. In the current study, reductions in pain medication usage by the yoga group of 25% were comparable to those reported with massage therapy (26%), chiropractic and physical therapy (24-27%), slightly greater than acupuncture (18%), and substantially larger than patient self-care (1%) (Skargren et al., 1997; Cherkin et al., 2001).
We can only compare the results of this study in a general way to those reported in the three published studies evaluating yoga on nonspecific CLBP because of differences in study design, measurement outcomes, instruments and yoga intervention. Present findings of decreased pain and improvement in functional disability following yoga reflect reported decreases in pain status (Vidyasagar etal., 1989) and improvement in disability (Galantino et.al. 2004) after yoga. Although Jacobs et al (2004) has some similar outcomes to the current study, they were not published at the time of submission of this manuscript. We expect differences in efficacy of Iyengar yoga from Jacobs et al. (2004) because a different selection of poses was used. The main difference in the Iyengar yoga intervention between the current study and the study by Jacobs et al (2004) is the lack of a resting phase of treatment prior to introducing more active poses and the inclusion of back bending poses in the later study.
The lack of treatment effect on the psychological and behavioral subscales is likely due to the study not having enough power to obtain statistical significance on these secondary outcomes. In addition, the duration of time necessary to change long-held negative cognitions and beliefs about CLBP such as movement-related fear, may be longer than the time required for improved perceptions of pain or disability. It is also possible that the inclusion of a large number of difficult standing postures that require repeated practice to obtain correct pelvic alignment diminished the efficacy of the intervention. Although BKS Iyengar (1976) claims that the standing poses are crucial for recovery from LBP, it is challenging to obtain the correct alignment in the posture that is necessary for pain relief in the learning phase. In such a short intervention, discomfort from improper alignment may have reduced the perceived efficacy of the yoga intervention on long-held negative cognitions and beliefs about the efficacy of yoga on CLBP. It is also possible that the impact of the yoga intervention would have been greater with a more experienced instructor.
The present study revealed methodological issues to address in future studies. In general, baseline measures for pain and functional disability were lower and ratings of back related self-efficacy were higher in the current study than many comparable studies in the literature for patients with CLBP (Grachev et al., 2002, McDonald and Weiskopf 2001; O’Sullivan et al., 1997; Wright et al., 2001). As a result, the study population was relatively healthy in terms of pain and functional disability and is likely due to the self-referral of subjects. This finding reduces the absolute magnitude of improvement due to border effects and limits the generalizability of the findings to less severe LBP populations. We recommend including cutoffs on outcome measures in the inclusion/ exclusion criteria so that a more disabled population is recruited and there is room for measuring improvement. We also recommend the use of fewer outcomes to increase the power of the study and to reduce demand characteristics, testing expectancies, or testing fatigue.
An additional major constraint of the study is the lack of control for attention and physical activity, both of which could be responsible for the significant effects observed in the yoga group. Thus, in future studies, in addition to a standard medical care control, a second control group should be included that controls for attention, group support and physical activity. It is also possible that the treatment effects could be due to therapist bias since the principal investigator of the study was also involved in the delivery of the yoga therapy intervention. We have attempted to minimize this bias by having the data collection and data analysis conducted by other members of the research team. The attrition in this study was twice as high as expected. In a study comparing the effect of medical exercise therapy to conventional physiotherapy and self-exercise, Torstensen et al. (1998) reported a 15.8% drop-out compared the 30% drop-out reported in this study. The attrition in this study drops to 18.3% when subjects are eliminated who discontinued in the study because they didn’t show up after the baseline assessment or turned out to be medically ineligible. In future studies, the attrition could be reduced by implementing a more rigorous physician screening to decreased the risk of medically ineligible subjects becoming enrolled in the study and by replacing subjects who don’t show up for the first session of treatment. We also believe that the efficacy of the yoga intervention would be enhanced by doing fewer and less challenging poses. We recommend excluding patients with symptomatic osteoarthritis to increase compliance to the yoga intervention and to decrease the likelihood of adverse reactions to the active yoga postures.
In spite of the aforementioned limitations, this pilot design demonstrated several methodological strengths. The current design used an objective and standardized screening process to randomize eligible subjects into a longitudinal, experimental design. Moreover, the experimental design incorporated a more realistic, active educational control condition rather than a passive wait-listed group in order to help maintain the motivation of this group and control for positive expectancy. In addition, subject assessment was multidimensional including both objective and subjective tests of disability, pain, and cognition, which enabled the researchers to better assess instruments and tests for a large scale, clinical trial. Potential confounding factors (age, gender, duration of LBP) were controlled for using an ANCOVA and by determining if there were differences between groups in medical and CAM treatment, and lifestyle changes that could account for the reported changes in pain-related outcomes. Although the duration of the yoga intervention was short by the standards of Iyengar yoga philosophy, significant results were manifested in a short time and adherence rates to yoga therapy were high. Poses and methods used for the treatment program were standardized and documented so that replication of the study is possible (Williams et al. 2003). Future studies should incorporate the above methodological changes. In addition, there is a need for clinical studies that determine whether yoga therapy can decrease medical utilization and for basic science studies that determine the mechanisms responsible for the therapeutic effects of Iyengar Yoga therapy on CLBP.
Acknowledgement
This project was funded by the Clinical Studies request for proposals at West Virginia University.
I would like to thank the following individuals who worked tirelessly to make this project a success: forth year physical therapy students (Sara Wigal, Cherie Straley, Erica Simpkins and Rebecca Wright) for preparing the newsletters for the educational control group and for performing the spinal range of motion measurements; Yoga teacher, Siegfried Bleher and student assistants (Lillian Waugh, Kathyrn Stedham, Suzie Luikhart) who helped deliver the yoga therapy intervention; Lori Stravers for screening subjects for eligibility; N. Noerachmanto for preparing figures, tables and references; Cathy Powell for her administrative assistance; Gerry Hobbs for overseeing the study design and statistical analysis.
Explore more from Yoga Vastu – Australia’s most progressive Iyengar Yoga resource
If you’re looking for relief of chronic back pain, Iyengar yoga could be exactly what your body is yearning for. While the benefits of yoga for lower back pain are vast, this healing practice can improve your mental health and overall wellbeing. If you’d like to try incorporating this into your day to day life, we recommend watching our Iyengar yoga videos for a range of step-by-step pose tutorials, short classes and full-length video sequences that’ll help support your practice. If you’d like to utilise our powerful way of learning, check out our yoga courses online or contact our instructors today.
References
- Anderson, K.O., Dowds, B.N., Pelletz, R.E., Edwards, W.T., Peeters-Asdourian, C. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain, Pain, 63 (1995) 77-84.
- Andersson, G., Epidemiological features of chronic low back pain, Lancet, 354 (1999) 581-585.
- Bombardier, C., Hayden, J., and Beaton, D.E., Minimal clinically important difference,
- Low back pain, outcome measures, J Rheumatol., 28 (2001) 431-438.
- Cherkin, D.C., Eisenberg, D., Sherman, K.J., Barlow, W., Kaptchuk, T.J., Street, J., Deyo, R.A., Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain, Arch Int. Med., 161 (2001) 1081-1088.
- Chibnall, J.T., and Tait, R.C., The Pain Disability Index: factor structure and normative data, Arch. Phys. Med. Rehabil., 75 (1994) 1082-1086.
- Crombez, G.J., Vlaeyen, W., Heuts, P.H. Lysens, R,Pain related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability, Pain, 80 (1999a) 329-339.
- Crombez, G., Eccleston, C., Baeyens, F., Van Houdenhove, B., Van den, B.A., Attention to chronic pain is dependent upon pain-related fear, J.Psychosom.Res., 47 (1999b) 403-410.
- Cohen, L., Warneke, C., Fouladi, R.T., Rodriguez, M.A., and Chaoul-Reich, A.,
- Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma, Cancer, 100 (2004) 2253-2260.
- Eisenberg, D.M., Davis, R.B., Ettner, S.L., Appel, S., Wilkey, S., Van Rompay, M., Kessler, R.C., Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey, JAMA, 280 (1998) 1569-1575.
- Eisenberg, D.M., Kessler, R.C., Foster, C., Norlock, F.E., Calkins, D.R., Delbanco, T.L., Unconventional medicine in the United States. Prevalence, costs, and patterns of use: N. Engl. J. Med., 328 (1993) 246-252.
- Frost, H., Klaber Moffett, J.A., Moser, J.S., Fairbank, J.C. Randomized controlled trial for evaluation of fitness program for patients with chronic low back pain, BMJ, 310 (1995) 151-154.
- Galantino, M.L., Bzdewka, T.M., Eissler-Russo, J.L., Holbrook, M.L., Mogck, E.P., Geigle, P., Farrar, J.T., The impact of modified Hatha yoga on chronic low back pain: a pilot study, Altern.Ther.Health Med., 10 (2004) 56-59.
- Garfinkel, M.S., Schumacher, H.R., Jr., Husain, A., Levy, M., and Reshetar, R.A., Evaluation of a yoga based regimen for treatment of osteoarthritis of the hands, J.Rheumatol., 21 (1994) 2341-2343.
- Garfinkel, M.S., Singhal, A., Katz, W.A., Allan, D.A., Reshetar, R., and Schumacher, H.R., Jr., Yoga-based intervention for carpal tunnel syndrome: a randomized trial, JAMA, 280 (1998) 1601-1603.
- Goubert, L., Francken, G., Crombez, G., Vansteenwegen, D., Lysens, R, Exposure to physical movement in chronic back pain patients: no evidence for generalization across different movements, Behav. Res. Ther., 40 (2002) 415-429.
- Grachev, I.D., Fredrickson, B.E. Apkarian, A.V. Brain chemistry reflects dual states of pain and anxiety in chronic low back pain, J Neural Transm., 109 (2002)1309-1334.
- Hagg, O., Fritzell, P., and Nordwall, A., The clinical importance of changes in outcome scores after treatment for chronic low back pain, Eur. Spine J., 12 (2003) 13-20.
- Huskisson, E.C., Visual Analogue Scales, In: R. Melzack (ed), Pain Measurement and Assessment, Raven Press, New York, 1983, pp 33-37.
- Iyengar,BKS, Light on Yoga, Schocken Books, New York, 1976.
- Iyengar, BKS, Tree of Yoga, Shambala, Boston, 1989.
- Iyengar National Association of United States (IYNAUS) Certification Committee, IYNAUS Certification Manual 2002.
- Jacobs, B.P., Mehling, W., Avins, A.L., Goldberg, H.A., Acree, M., Lasater, J.H., Cole, R.J., Riley, D.S., Maurer, S. Feasibility of conducting a clinical trial on Hatha yoga for chronic low back pain: methodological lessons, Altern.Ther.Health Med., 10 (2004) 80-83.
- Jensen, M.P., Turner, J.A., Romano, J.M., Lawler, B.K., Relationship of pain-specific beliefs to chronic pain adjustment, Pain, 57 (1994) 301-309.
- Jensen, M.P., Turner, J.A., Romano, J.M. Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment, JConsult Clin. Psychol., 69 (2001) 655-662.
- Jerome, A., Gross, R.T., Pain disability index: construct and discriminant validity, Arch. Phys. Med. Rehabil., 72 (1991) 920-922.
- Kankaapää, M., Taimela, S., Airaksinen, O., Hanninen, O., The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self-experienced disability, and lumbar fatigability, Spine, 24 (1999) 1034-1042.
- Kori, S.H., Miller, R.P., Todd, D.D., Kinisophobia: a new view of chronic pain behavior: Pain Manag., (1990) 35-43.
- Lethem, J., Slade, P.D., Troup, J.D., Bentley, G. Outline of a Fear-Avoidance Model of exaggerated pain perception – I, Behav. Res. Ther., 21 (1983) 401-408.
- Mayer, T.G., Kondraske, G., Beals, S.B., Gatchel, R.J. Spinal range of motion. Accuracy and sources of error with inclinometric measurement, Spine, 22 (1997) 1976-1984.
- McCracken, L.M., Zayfert, C., Gross, R.T., The Pain Anxiety Symptoms Scale: development and validation of a scale to measure fear of pain, Pain, 50 (1992) 67-73.
- McDonald, D.D., and Weiskopf, C.S. Adult patients’ postoperative pain descriptions and responses to the Short-Form McGill Pain Questionnaire, Clin.Nurs.Res., 10 (2001) 442-452.
- Melzack, R., The short-form McGill Pain Questionnaire, Pain, 30 (1987) 191-197.
- Morley, S., Eccleston, C., and Williams, A., Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache , Pain, 80 (1999) 1-13.
- Murugesan, R., Govindarajulu, N., and Bera, T.K., Effect of selected yogic practices on the management of hypertension, Indian J. Physiol Pharmacol., 44 (2000) 207-210.
- Nagarathna, R. and Nagendra, H.R., Yoga for bronchial asthma: a controlled study, Br. Med. J.(Clin.Res.Ed), 291 (1985) 1077-1079.
- O’Sullivan, P.B., Phyty, G.D., Twomey, L.T. Allison, G.T. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis, Spine, 22 (1997) 2959-2967.
- Oken, B.S., Kishiyama, S., Zajdel, D., Bourdette, D., Carlsen, J., Haas, M., Hugos, C., Kraemer, D.F., Lawrence, J., and Mass, M., Randomized controlled trial of yoga and exercise in multiple sclerosis, Neurology, 62 (2004) 2058-2064.
- Risch, S.V., Norvell, N.K., Pollock, M.L., Risch, E.D., Langer, H., Fulton, M., Graves, J.E., and Leggett, S.H., Lumbar strengthening in chronic low back pain patients. Physiologic and psychological benefits, Spine, 18 (1993) 232-238.
- Riley III, J.L., Robinson, M.E., CSQ: five factors or fiction?, Clin.J Pain, 13 (1997) 156-162.
- Robinson, M.E., Riley, III, J.L., Myers, C.D. Sadler, I. J., Kvaal, S.A., Geisser, M.E., Keefe, F.J., The Coping Strategies Questionnaire: a large sample, item level factor analysis, Clin. J Pain, 13 (1997) 43-49.
- Saper, R.B., Phillips, R.S., Davis, R.B., Eisenberg, D.M., Prevalence and Patterns of Hatha Yoga Use in the United States, Poster presented at International Scientific Conference on Complementary, Alternative and Integrative Medicine Research April 12-14[Boston: MA] 2002.
- Shaffer, H.J., LaSalvia, T.A., and Stein, J.P., Comparing Hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial, Altern.Ther.Health Med., 3 (1997) 57-66.
- Shelerud, R., Epidemiology of occupational low back pain, Occup.Med., 13 (1998) 1-22.
- Signet Market Research. Yoga Survey 2000. Yoga Journal. 2000.
The original article has been published in Pain (2005) 115: 107-117.